ARTICLES, DRUG ABUSE & EFFECTS OF ALCOHOL. REHABILITATION
Overdose Survival Guide
Overdose Prevention and Response
It’s important to recognize an overdose and know what to do when it happens. Here’s a guideline to help you take the right actions and how to treat it before it’s too late.
Overdose is Most Common When:
- Your tolerance is lower: you took a break, were in detox/treatment or jail, or you are new to use
- You have been sick, tired, run down, dehydrated or have liver issues
- You mix drugs: prescribed or not, legal or illegal
- The drugs are stronger than you are used to: changes in supply, dealer, or town
To Prevent Overdose:
- Know your health status and your tolerance
- Be aware: using drugs while on prescribed medications can increase overdose risk
- Don’t use alone. Leave the door unlocked. Tell someone to check on you
- Do testers to check strength. Use less. Pace yourself
- Talk to an experienced person or a trusted healthcare provider about reducing risk
- Know CPR and get trained on giving naloxone
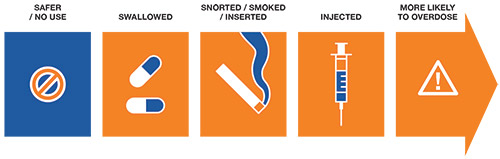
- Choose a safer route of taking drugs
Choose a Safer Route
The Recovery Position
Keep the Airway Clear
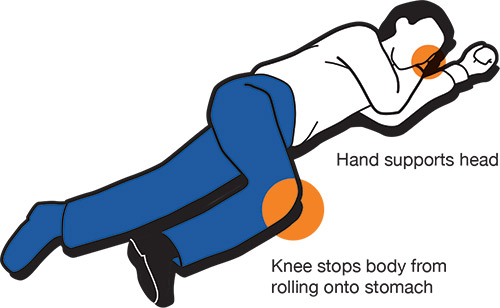
Stay with the person. If you must leave them alone at any point, or if they are unconscious, put them in this position to keep airway clear and prevent choking.
Overdose? Take Charge. Take Care.
Opioids/Depressants
(e.g., opioids: morphine, Dilaudid, heroin/depressants: alcohol, GHB, benzodiazepines)
Feels and Looks Like:
- Person cannot stay awake
- Can’t talk or walk
- Slow or no pulse
- Slow or no breathing, gurgling
- Skin looks pale or blue, feels cold
- Pupils are pinned or eyes rolled back
- Vomiting
- Body is limp
- No response to noise or knuckles being rubbed hard on
the breastbone
In Case of an Opioid Overdose:
- Stay with the person. Use their name. Tell them to breathe
- Call 911 and tell them the person is not breathing. When paramedics arrive, tell them as much as you can about drugs and dose
- Use naloxone if available. Naloxone only works on opioid overdoses
- After administering naloxone, a person might feel withdrawal. Do not let them take more drugs. The sick feeling will go away when naloxone wears off (30 – 75 minutes). Be aware: the overdose can return
Save ME
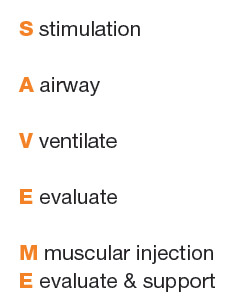
Can you wake them up?
If not, call 911
Make sure there’s nothing in their mouth that stops them from breathing.
Breathe for them. (Plug nose, tilt head back, and give 1 breath every 5 secs).
Are they any better?
Are you trained to give naloxone?
Inject 1cc of naloxone into a muscle.
Is the person breathing on their own?
If they’re not awake in 5 min, another
1cc dose is needed. Tell the person not to use any more drugs right now and wait at least 2 hours.
This is proven to work. Other remedies can actually be harmful.
—
Stimulants
(e.g., cocaine, methamphetamine, ecstasy)
Feels and Looks Like:
- Fast pulse or no pulse
- Short of breath
- Body is hot/sweaty, or hot/dry
- Confusion, hallucinations, unconscious
- Clenched jaw
- Shaky
- Chest pain
- Seizures
- Vomiting
- Cannot talk or walk
There are NO medications to safely reverse a stimulant overdose.
Assessment: Are They Experiencing A or B?
A: Mental Distress/ Overamp
Associated with: sleep deprivation, crashing, anxiety, paranoia. If a person is conscious, and you are sure this is not medical in nature, they may just need support and rest. Call Poison Control to help assess.
What to do:
- Keep calm. Stay with the person. Use their name
- Give water or fluid with electrolytes. Do not overhydrate
- Place cool, wet cloths under armpits, back of neck, and head
- Open a window for fresh air
- Get them comfortable. Move away from activity
- If aggressive/ paranoid suggest they close their eyes, give person space
- Encourage person not to take any other substances
- Doctor may treat agitation and paranoia with a benzodiazepine
If you’re not comfortable with the situation, call 911.
B: Physical Distress/Acute Stimulant Toxicity
Medical attention is required immediately if a person has:
- Jerking or rigid limbs
- Rapidly escalating body temperature and pulse
- In and out of consciousness
- Severe headache, sweating, agitation
- Chest pains
What to do:
- Call 911
- Stay with person
- Keep person: conscious, hydrated, calm
- If heart has stopped do ‘hands-only’ CPR
- Tell medical professionals as much as possible so they can give the right treatment to prevent organ damage and death